05.08.2025
Article
2024 Patient Safety and Quality Benchmark Report
The 2024 Patient Safety and Quality Benchmark Report provides a comprehensive analysis of healthcare facilities' performa...
Learn MoreEvery MIPS point will help you earn your fair share of the possible incentive money this year. In the CY 2021 PFS Final Rule, CMS states that with the finalized “performance threshold at 60 points, the maximum payment adjustment is 7.36 percent. However, if you ignore MIPS, your efforts aren’t a priority or you slack off, you could be penalized up to -9%.
Let’s talk about what can you do in each category to stay on track and protect your reimbursement.
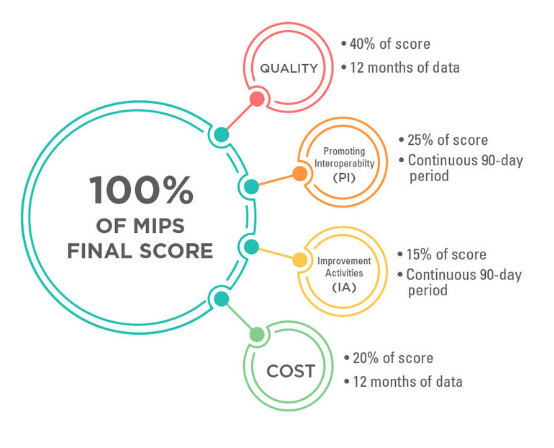
This is your biggest opportunity to increase your score and do well by monitoring your quality measure performance. Check reports at least bi-weekly to ensure you are closing the gaps in capturing data. Use the reports to guide feedback to the eligible clinicians and staff in your organization who collect the data.
Don’t lose sight of data completeness. CMS maintains a 70% data completeness requirement. This means you need to report performance or exclusion/exception data for at least 70% of the patients and/or encounters that are eligible for the measure’s denominator. To succeed in this, you’ll need to ensure you gather each applicable measure, every encounter, for every patient to ensure data completeness is reached.
The PI category contains multiple measures. The scoreless pre-requisites of this category are one of the key items many groups and clinicians lose sight of. CMS requires you to sign off on information blocking statements as well as those confirming you have completed your annual MIPS compliant Security Risk Assessment (SRA).
Neither of these tasks is performed by your EHR vendor and remain the inherent responsibility of each practice.
Like Quality, you will want to ensure your practice runs reports for PI measures. If you have any undesirable or non-compliant measure performance, check the measure’s requirements and be sure to work on improving now before the hustle and bustle of holidays and year-end activities kick into full gear. The best gift you can give yourself is to allow ample time for remediation and to ensure you maximize this category’s points.
Improvement Activities only require 90 days of performance data and are often represented by a simple checkbox for many clinicians and practices. If you report as a group, more than 50% of the eligible clinicians in your practice must perform the activity.
Documentation is key for any activity. Be sure you maintain proof of the activity performed, who participated in it, and with as much detail as possible, how it was carried out.
While it may feel like your work is done when the clock strikes midnight on December 31, the time will soon come to report all this data after the new year.
Again, remember to document ALL your efforts in the event of an audit. We recommend keeping your final Quality and PI reports for the year, relevant screenshots, any process documentation, and even your notes. These can all be helpful if an audit ever comes to bear, which can happen for up to six years after submission.
05.08.2025
Article
The 2024 Patient Safety and Quality Benchmark Report provides a comprehensive analysis of healthcare facilities' performa...
Learn More
07.11.2024
Article
Here's how implementing return-to-work programs benefits healthcare organizations.
Learn More
07.11.2024
Article
Explore Section 111 mandatory reporting requirements and how LHA Trust Funds can assist with compliance.
Learn More